Cervical Disc Arthroplasty for Multi-Level Degeneration: Is It Possible?
Degenerative disc disease in the cervical spine can be debilitating, causing chronic neck pain, stiffness, and radiating symptoms into the shoulders and arms. Traditionally, spinal fusion has been the go-to treatment for severe cases. However, in recent years, cervical disc arthroplasty (CDA)—also known as artificial disc replacement—has emerged as a motion-preserving alternative.
While single-level cervical disc replacement is now well-established and FDA-approved, a growing number of patients are asking: Can cervical disc arthroplasty be performed at multiple levels? The answer is yes—but with important considerations.
In this blog, we’ll explore what cervical disc arthroplasty is, the challenges and opportunities in multi-level procedures, and who may be a candidate for this cutting-edge surgical solution.
What Is Cervical Disc Arthroplasty?
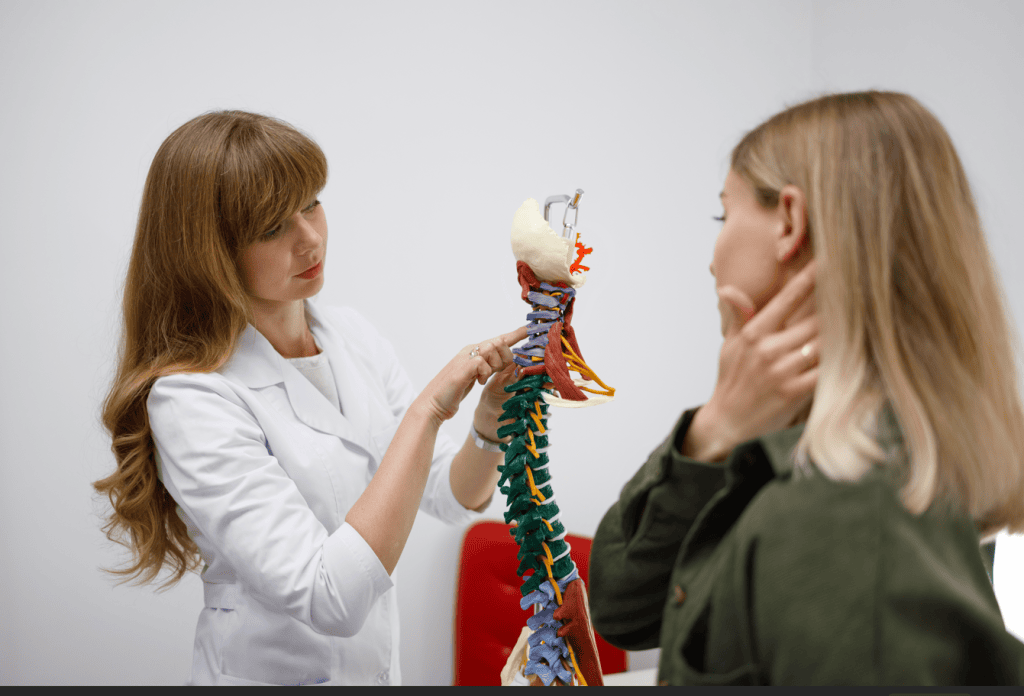
Cervical disc arthroplasty is a surgical procedure designed to replace a damaged or degenerated cervical disc with an artificial one. This artificial disc maintains motion between the vertebrae, unlike fusion surgery, which permanently immobilizes the segment.
The procedure aims to:
- Relieve nerve compression
- Reduce pain and neurological symptoms
- Preserve spinal motion and function
- Reduce the risk of adjacent segment disease (ASD)
The artificial disc typically consists of metal and polymer components designed to mimic the natural motion of a healthy disc.

Understanding Multi-Level Degenerative Disc Disease
Multi-level cervical disc degeneration involves wear-and-tear or injury affecting two or more discs in the neck. Common causes include:
- Age-related degeneration
- Repetitive strain or poor posture
- Genetic predisposition
- Trauma or herniated discs
Symptoms may include:
- Chronic neck pain
- Numbness or tingling in the arms
- Weakness in hands or shoulders
- Decreased range of motion
When conservative treatments (physical therapy, medications, injections) fail, surgery may be necessary.

Traditional Approach: Multi-Level Anterior Cervical Discectomy and Fusion (ACDF)
For decades, multi-level ACDF has been the gold standard. In this procedure, the damaged discs are removed, and the vertebrae are fused using bone grafts and plates.
While effective in relieving symptoms, fusion has some limitations:
- Loss of motion at the operated levels
- Potential for hardware-related complications
- Increased stress on adjacent levels, leading to adjacent segment disease (ASD)
- Longer recovery times
These drawbacks have led to increasing interest in motion-preserving alternatives like cervical disc arthroplasty.
The Rise of Multi-Level Cervical Disc Arthroplasty
Originally approved for single-level disc disease, cervical disc arthroplasty has shown promising results for selected cases involving two or more levels. In fact, some artificial disc devices are now FDA-approved for two-level replacement (e.g., the Mobi-C®, Prestige LP®).
Advantages of Multi-Level CDA:
- Preservation of motion at operated segments
- Lower incidence of ASD compared to fusion
- Faster return to activity in many patients
- Improved long-term neck mobility
- No need for bone grafts or spinal fusion
These benefits have led to increased demand among patients seeking a less invasive, more dynamic solution to cervical disc disease.
What Does the Research Say?
Several studies and clinical trials have examined the safety and effectiveness of multi-level CDA. Here are some key findings:
- A 2020 study in The Spine Journal compared two-level CDA to two-level ACDF and found that CDA patients had lower rates of reoperation, faster recovery, and higher satisfaction scores.
- The FDA IDE (Investigational New Drug) study for the Mobi-C® disc showed that two-level CDA was not inferior to ACDF, and in many measures, outperformed fusion at 5-year follow-up.
- Other trials report lower complication rates, preserved spinal kinematics, and better quality of life metrics in multi-level CDA patients.
These results support the growing acceptance of multi-level CDA in the surgical community, though it’s not suitable for everyone.

Who Is a Candidate for Multi-Level CDA?
Not every patient with multi-level cervical degeneration is a good candidate for arthroplasty. Ideal candidates typically include:
- Patients with degenerative disc disease or herniated discs at 2 (occasionally 3) contiguous levels
- Those with preserved facet joint health
- Patients without severe cervical instability or deformity
- Individuals who have failed conservative treatment (e.g., physical therapy, medications)
- Patients without advanced osteoporosis or infection
Preoperative imaging (MRI, CT, X-rays) is essential to evaluate disc height, alignment, and the health of adjacent structures.
Contraindications may include:
- Severe osteoporosis
- Active infection
- Cervical instability or kyphosis
- Facet joint arthritis
- Allergy to implant materials
The Surgical Process
Multi-level cervical disc arthroplasty is usually performed under general anesthesia. The surgeon makes a small incision in the front of the neck, removes the degenerated discs, decompresses the spinal cord and nerves, and inserts the artificial discs.
The entire procedure may take 2–4 hours, depending on the number of levels treated. Most patients are discharged within 1–2 days and begin physical therapy shortly after.
Recovery and Outlook
Recovery from multi-level CDA is generally quicker than multi-level fusion. Patients often experience:
- Less post-operative stiffness
- A quicker return to work and daily activities
- Sustained symptom relief over time
- Improved neck mobility
Most patients can resume light activities within 2–4 weeks and return to full activity within 2–3 months. Long-term follow-ups show continued motion preservation and minimal complications in properly selected patients.
The Future of Multi-Level Disc Replacement
While two-level disc arthroplasty is now more widely accepted, three-level CDA is still considered experimental or off-label in most cases. Some spine surgeons are cautiously exploring three-level replacements in highly selective scenarios with promising early results.
Ongoing innovations in implant materials, surgical techniques, and biomechanical modeling are likely to expand the indications for multi-level CDA in the years to come.
Conclusion
Cervical disc arthroplasty is no longer just for single-level disease. Multi-level CDA is a viable and increasingly popular option for patients with degenerative disc disease affecting two adjacent cervical levels. It offers the promise of pain relief without compromising motion, a quicker recovery, and a reduced risk of adjacent segment issues.
However, patient selection remains critical. A thorough evaluation by an experienced spine surgeon, supported by imaging and diagnostic studies, is essential to determine if you’re a candidate for multi-level cervical disc replacement.
As with any medical decision, it’s important to discuss all available options—fusion, arthroplasty, or hybrid approaches—with your healthcare provider to find the best path forward for your spine health.