Avoiding Adjacent Segment Disease: The Advantage of Arthroplasty Over Fusion
Spinal surgery has evolved dramatically over the past few decades, offering patients relief from debilitating conditions like degenerative disc disease, herniated discs, and spinal instability. Traditionally, spinal fusion has been the go-to surgical solution, particularly in the cervical and lumbar regions. While effective in stabilizing the spine and alleviating pain, spinal fusion carries a significant long-term risk: Adjacent Segment Disease (ASD).
With advances in motion-preserving technologies, arthroplasty—also known as artificial disc replacement—has emerged as a compelling alternative. One of its most promising benefits? A lower risk of ASD. In this post, we’ll explore what adjacent segment disease is, why fusion increases the risk, and how arthroplasty helps prevent it.
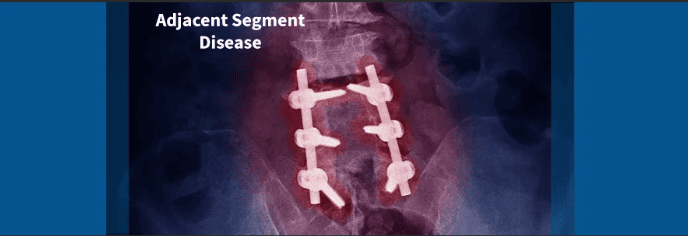
What Is Adjacent Segment Disease?
Adjacent Segment Disease (ASD) refers to the accelerated degeneration of the spinal discs and joints directly above or below a spinal fusion site. This phenomenon occurs when the fused segment can no longer move, forcing adjacent segments to absorb increased mechanical stress.
Common symptoms of ASD include
- New or worsening back or neck pain
- Radiating arm or leg pain (radiculopathy)
- Neurological symptoms such as weakness or numbness
- Decreased mobility or spinal stiffness
In many cases, ASD leads to additional surgeries, compounding patient recovery time and healthcare costs.

Why Does Spinal Fusion Cause ASD?
Spinal fusion works by eliminating movement at a problematic spinal segment, typically using bone grafts and hardware like screws and rods. This can effectively relieve pain by stabilizing the spine, but it changes the spine’s natural mechanics.
How fusion contributes to ASD:
- Loss of motion: The fused vertebrae become one immobile unit.
- Increased load: Adjacent segments compensate by moving more, which increases wear and tear.
- Accelerated degeneration: Over time, this extra stress leads to disc breakdown, facet joint arthritis, and nerve compression.
Clinical studies suggest that ASD occurs in up to 25% of patients within 10 years after fusion surgery, with many requiring revision procedures.
Arthroplasty: A Motion-Preserving Alternative
Arthroplasty, or artificial disc replacement, is a modern surgical option that aims to relieve spinal pain while maintaining motion at the treated level. Instead of fusing the vertebrae, the damaged disc is removed and replaced with a mechanical implant that mimics the function of a healthy disc.
Benefits of arthroplasty:
- Preserves natural spinal movement
- Maintains normal load distribution
- Reduces stress on adjacent segments
- Decreases the risk of ASD
The fundamental goal of arthroplasty is to treat the problem without altering spinal biomechanics—a key factor in preventing long-term degeneration.
What the Research Says
A growing body of scientific literature supports the advantage of arthroplasty over fusion in preventing adjacent segment disease.
Key findings:
- A landmark FDA-approved study comparing cervical disc replacement with fusion found significantly lower reoperation rates at adjacent levels in the arthroplasty group.
- Long-term follow-ups (10+ years) indicate fewer cases of ASD in patients who received disc replacements.
- Patients who undergo arthroplasty tend to maintain better range of motion and report higher satisfaction post-operatively.
A 2021 meta-analysis in The Spine Journal concluded that arthroplasty offers superior outcomes in terms of ASD prevention, mobility, and overall patient function when compared to fusion.
Who Is a Candidate for Arthroplasty?
While arthroplasty offers many advantages, it’s not suitable for every patient. Proper candidate selection is crucial for long-term success.
Ideal candidates:
- Age 20–60 with a single-level or two-level disc disease
- No significant facet joint degeneration
- Good bone quality (no severe osteoporosis)
- No spinal deformity or instability
- Normal alignment of the spine
Not ideal candidates:
- Severe arthritis or spondylolisthesis
- History of spinal infection or tumors
- Previous spinal fusion at the same level
- Osteoporotic bones
A comprehensive evaluation, including X-rays, MRI, and sometimes CT scans, helps surgeons determine eligibility.
Hybrid Surgery: A Balanced Approach
In patients with multi-level degeneration, hybrid surgery—combining fusion at one level and arthroplasty at another—can provide an effective solution. This approach allows for
- Motion preservation at suitable levels
- Stabilization where necessary
- Reduced risk of ASD at non-fused segments
Hybrid constructs are becoming increasingly common as surgeons aim to optimize long-term outcomes and minimize complications.
The Cost of ASD: Physical, Emotional, and Financial
Adjacent Segment Disease doesn’t just result in medical complications—it affects quality of life:
- Physical toll: Chronic pain, limited mobility, and reduced activity
- Emotional burden: Anxiety, depression, and frustration from recurrent issues
- Financial strain: Additional surgeries, rehabilitation, lost wages
By preserving motion and spinal mechanics, arthroplasty helps patients avoid these challenges, offering a more durable solution in the right clinical setting.

The Future of Spinal Surgery
With ongoing advancements in implant design, materials, and surgical techniques, arthroplasty is poised to become the new standard for appropriately selected patients.
Innovations such as
- Biomimetic disc implants
- 3D-printed prosthetics
- Robotic-assisted implantation
…are all making the procedure more precise, customizable, and accessible.
Conclusion
Spinal fusion has helped millions of people regain function and live pain-free lives. However, it comes with the long-term risk of adjacent segment disease—a complication that can undermine surgical success.
Arthroplasty offers a compelling alternative by preserving motion, maintaining normal spine biomechanics, and dramatically reducing the likelihood of adjacent segment breakdown. While not suitable for every patient, those who meet the criteria can benefit from improved outcomes and a lower chance of future surgery.
If you’re facing spinal surgery, ask your spine specialist about the risks of ASD and whether disc replacement might be right for you. With the right procedure, you can move forward—literally and figuratively—toward a healthier spine and a better quality of life.
